CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD)
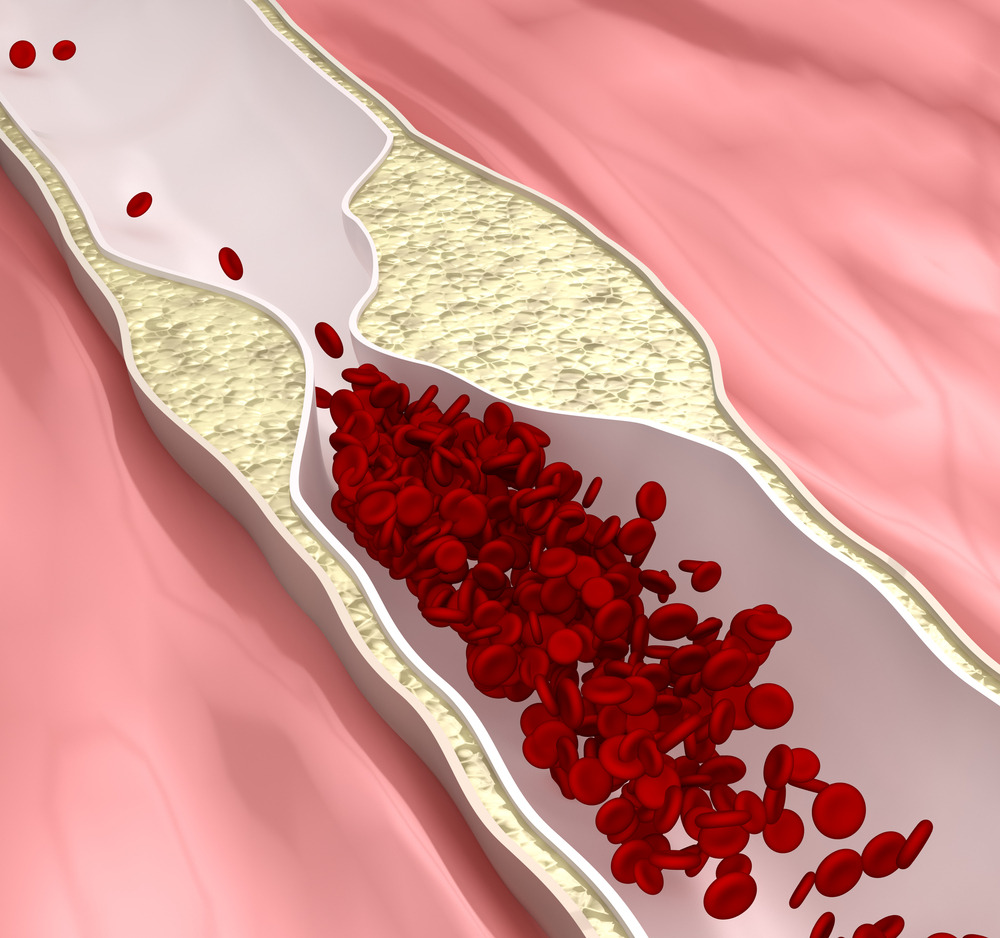
DEFINITION: Is a
disease state in which airflow is obstructed by emphysema, chronic bronchitis
or both. The airflow obstruction is usually progressive, irreversible, and
associated with airway hyperactivity, resulting in narrowing of peripheral
airways, airflow limitation and changes in the pulmonary vasculature.
RISK FACTORS:
cigarette smoking, air pollution and occupational exposure(coal, cotton and
grain)
CLINICAL MANIFESTATIONS:
· Dyspnea, cough
and increased work of breathing
·
Dyspnea on mild exertion
advancing to dyspnea at rest
· Weight loss
· Symptoms
are specific to disease: Bronchitis and Emphysema
SYMPTOMS:
BRONCHITIS-
· Chronic
cough and production of copious purulent sputum which has a quality of layering
out into three layers on stranding, a frothy top layer, a middle clear layer
and a dense particular layer,
· hemoptysis,
clubbing of the fingers and
· repeated
episodes of pulmonary infection.
EMPHYSEMA-
· Dyspnea
with insidious onset progressing to severe dyspnea with slight exertion.
· Chronic
cough, wheezing, dyspnea, fatigue, and tachypnea
· On
inspection “barrel chest” due to air traping, muscle wasting and pursed lip
breathing
· On
auscultation, diminished breath sounds with crackles, wheezes, rhonchi and
prolonged expiration
·
Hyperresonance with percussion and a decrease in fremitus
· Anorexia, weight loss, weakness and
inactivity
· Hypoxemia
and Hypercapnia, morning headache in advance stages
·
Inflammatory reactions and infections from pooled secretions.
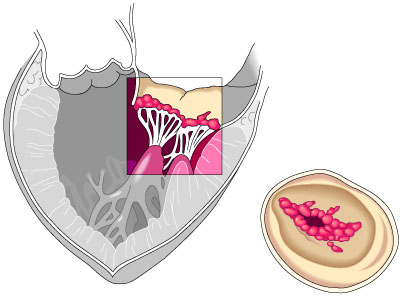
COMPLICATIONS:
· Respiratory
insufficiency or failure
· Atelectasis
· Pneumonia
·
Pneumothorax
· Pulmonary
HPN
Medical management:
·
Bronchodilators
· Oxygen
Therapy including nighttime oxygen
· Varied
treatment specific to disease
NURSING MANAGEMENT:
I.ASSESSMENT
· Assess risk factors
· Obtain
health history such as duration of respiratory difficulty, dyspnea, shortness
of breath, wheezing, exercise, tolerance, fatigue, effects on eating and
sleeping habits
· Perform
physical examination to obtain baseline data:
- Pulse, RR, and rhythm
- Contraction of
abdominal muscles during inspiration
- Use of
accessory muscles to breathe, prolonged expiration
- Cyanosis, neck
vein engorgement
- Peripheral
edema
- Cough, color,
amount and consistency of sputum
- Status of
sensorium, increasing stupor, apprehension
II. NURSING DIAGNOSIS
· Impaired
gas exchange related to ventilation perfusion inequality
· Ineffective
airway clearance related to bronchoconstriction, increased mucus production,
ineffective cough and bronchopulmonary infection.
· Ineffective
breathing pattern related to shortness of breath, mucus, bronchoconstiction and
airway irritants
· Self- care
deficit related to fatigue secondary to increased work of breathing and
insufficient ventilation and oxygenation.
· Activity
intolerance due to fatigue, hypoxemia and ineffective breathing pattern
· Ineffective
coping related to less socialization, anxiety, depression, lower activity level
and inability to work
· Deficient
knowledge related to risk of smoking as evidenced by continuing at risk
behaviors
III.
PLANNING
· Improved
gas exchange
· Smoking
cessation
· Improved
breathing pattern
· Maximal
self- management
· Improved
activity tolerance
· Achievement
of airway clearance
· Impaired
coping ability
· Improved
health related quality of life
· Adherence
to the therapeutic programs and home care
IV NURSING INTERVENTIONS:
Improving Gas Exchange
· Monitor
Dyspnea and Hypoxia
· Administer
Medications and be alert for potential
side effects
· Assess
relief of bronchospasm through patient report of less dyspnea
· Monitor
prescribed oxygen effectiveness with pulse oximetry or arterial blood gas (ABG
) analysis
Achieving Airway Clearance
· Encourage
high fluid intake to liquefy secretions
· Instruct patient in directed or
controlled coughing
· Provide
chest physiotherapy with potential drainage and intermittent passive pressure
(IPPB) when ordered
· Instruct
patient in effective breathing techniques
· Measure expiratory
flow rates
Preventing
Bronchopulmonary Infections
· Instruct patient to report signs of
infection and report any worsening of symptoms
· Advise
patient to avoid outdoor exposure during high pollen counts or significant air pollution
because there may increase bronchospasm
· Encourage
immunization against hemophilus Influenzae and streptococcus pneumonia and
pneumococcal vaccine every 5 to 7 yrs.
IV. EVALUATION:
Expected patient
outcomes:
· Demonstrates
improved gas exchange
· Achieves
maximal airway clearance
· Improves
breathing pattern
· Maintains
maximal level of self-care and physical functioning
· Achieves
activity tolerance and exercises and performs activities with less shortness of
breath
· Develops
effective coping mechanisms and participates in a pulmonary rehabilitation
program
· Adheres to
the therapeutic program